What is an intra-uterine device?
An intra-uterine device (IUD) is placed inside the uterus (womb) to prevent pregnancy.
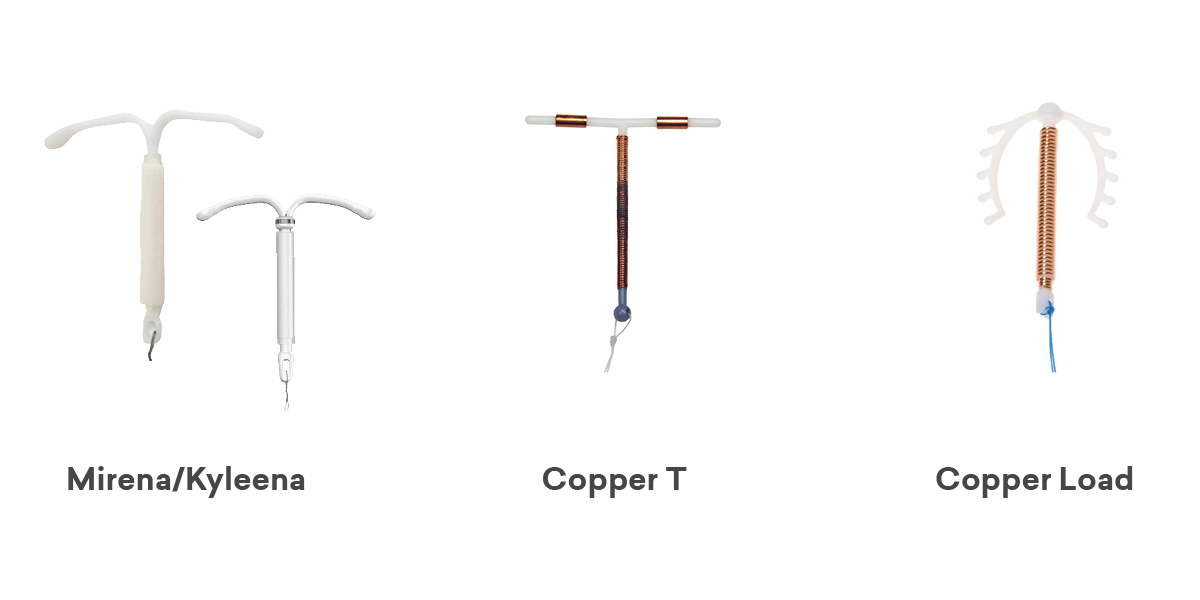
At SHINE SA two types of IUD are used:
- hormonal IUDs (Mirena and Kyleena) made of plastic that releases small amounts of progestogen into the uterus
- copper IUDs (Load and Copper T) made of plastic and copper
IUDs are Long Acting Reversible Contraceptives (LARCs) meaning they are long acting and don’t require you to do anything to prevent pregnancy every day or every time you have sex. LARCs are the most effective contraception methods (greater than 99% effective) and are suitable for most people. LARCs do not have any impact on fertility, when they are stopped fertility returns to normal immediately.
How do IUDs work?
Copper IUDs affect sperm movement to the egg and change the lining of the uterus to make it difficult for a fertilised egg to take hold.
Hormonal IUDs thicken the mucus at the neck of the uterus, blocking the sperm. They may also affect ovulation by changing the hormones that cause an egg to be released each month.
How can I get an IUD?
If you decide to use an IUD you will usually need to have an appointment to discuss what type of IUD suits you. An IUD may not be suitable for a small number of people and this may mean you are recommended to use a different form of contraception. If an IUD is suitable, you can then make an appointment to get an IUD inserted. You may need to purchase the IUD and bring it with you to your appointment.
What are the benefits of having an IUD?
- They are a very effective, reliable method of contraception (greater than 99% effective) and work for a long time. Copper IUDs are effective for 5 or 10 years depending on the type. Hormonal IUDs are effective for 5 years.
- They are a ‘set and forget’ method.
- They can be taken out at any time and they are easily removed.
- They are fully reversible, fertility is considered returned as soon as the IUD is removed.
- Copper IUDs (Load and Copper T) can be used as highly effective emergency contraception.
- The Mirena IUD can be used to treat heavy menstrual bleeding.
- The Mirena IUD can be used as part of menopause hormone treatment.
What are the side effects?
The side effects and complications with all IUDs include:
- a small risk of developing pelvic infection in the first 3 weeks following insertion (this is easily treated with antibiotics)
- a small risk of perforation of the uterus during insertion
- a small risk of the IUD moving from its position or coming out (expulsion)
- a very small risk of ectopic pregnancy (pregnancy developing in the tubes)
People using copper IUDs may have:
- spotting, heavier and/or longer periods, which may settle after the first 3–6 months
People using hormonal IUDs may have:
- persistent or irregular bleeding and/or spotting for the first 3–5 months
- no periods at all or occasional light periods by 12 months
- hormonal side effects are rare and can include hair change, acne, headache and breast tenderness, which usually settle after the first 3 months
- ovarian cysts may occur when using the hormonal IUD; however, most cysts will not cause pain and will settle without any treatment
Who should not use IUDs?
IUDs may not be suitable for people:
- who have a current sexually transmitted infection
- with abnormal vaginal bleeding (this may need to be checked by a doctor first)
- with certain known abnormalities of the uterus such as large fibroids
A copper IUD may not be your first choice of contraception if you have:
- heavier periods
- anaemia (low blood iron)
The hormonal IUD is not recommended for people with past or current breast cancer.
When can an IUD be inserted?
Hormonal IUDs should be inserted during the first 7 days of your menstrual cycle, which starts with the first day of bleeding.
Copper IUDs should be inserted during the first 12 days of your menstrual cycle, which starts with the first day of bleeding.
If inserted at any other time in the cycle then pregnancy needs to be completely excluded.
If you are using other methods of contraception and are changing to an IUD you need to discuss with the doctor when the IUD should be inserted.
To decrease cramping a medicine used for period pain, such as Nurofen, Ponstan or Naprogesic, should be taken one hour before insertion.
Make sure you have eaten breakfast or lunch on the day the IUD is being inserted and have drunk plenty of fluids.
When does the IUD start working?
If the IUD is inserted as recommended above, the contraceptive effect will start immediately. It may be inserted at another time in the cycle if pregnancy can be ruled out; in that case it will be effective after 7 days.
When can an IUD be used after childbirth?
An IUD can be inserted from 4-6 weeks after childbirth.
What do I do after my IUD has been put in?
To reduce the risk of infection, avoid sex, tampons, swimming and baths for 48 hours after insertion.
If cramps occur, take medicine used for period pain to reduce pain and the risk of the IUD coming out. Heat packs can also be beneficial to reduce cramping.
You should check your IUD strings about 1 week after insertion. People using copper IUDs are recommended to check their strings after every period. To check that your IUD is still in place insert one or two fingers into your vagina to feel the string.
Contact your doctor or SHINE SA if you:
- cannot feel the string
- feel the string has lengthened
- can feel the hard stem of the IUD
Use another form of contraception (e.g. a condom) until you have had a check-up.
You should also contact your doctor or SHINE SA if you have any of the following symptoms:
- a fever or you’re feeling unwell, weak or tired
- persistent or excessive cramps or back pain
- unusual pelvic pain or tenderness
- unusual vaginal discharge or odour
- pain during sex
If you have a copper IUD and your period is more than a week overdue you should do a pregnancy test or see your doctor/SHINE SA.
You will need to have a check-up by 6 weeks or if you have any concerns at any time.
When can the IUD be removed?
An IUD can be removed at any time but there is a risk of pregnancy if you have had unprotected sexual intercourse within the last week. It’s a good idea to use condoms or avoid sex for 7 days before removal, unless you are planning a pregnancy.
Looking for a practitioner to help you with getting an IUD?
This list is provided to assist you in finding an IUD inserting practitioner outside of SHINE SA.
South Australian IUD Inserters List






